Dr Steel has been practicing and teaching minimally invasive spine surgery techniques as a consultant for 16 years. He routinely uses minimally invasive techniques and percutaneous approaches for all patients in whom it is suitable. In some cases, a person’s condition makes keyhole spine surgery impossible. This is discussed with each patient on an individual basis at the time of consultation.
Minimally Invasive Spine Surgery helps to minimise post-operative pain, allows patients to be discharged from hospital earlier, and return to their normal activities sooner because there is less disruption to the spinal muscles.
Minimally Invasive Spine Surgery (MISS) means using the smallest incision and exposure or access port possible. Dr Steel helped pioneer the use of minimally invasive techniques in spine surgery and uses them on virtually all his patients. This allows less pain, fewer complications and faster recovery from the surgery. Many Patient can even go home the day of their operation.
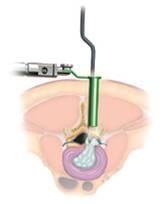
Dr Steel performs this surgery by using x-ray guidance and stereotactic navigation to make one or more small incisions to gain access to the spine. He forms a tunnel by passing dilating tubular retractors down to the area of the spine that needs to be operated on. When the final retractor is secured Dr Steel uses specialised bayoneted instruments and a microscope to perform the surgery.
Minimally invasive spine surgery can range from decompressions and discectomies through to multi-level instrumented spine fusions and corrective reconstruction. In comparison, traditional open spine surgery require a bigger incision and more disruption to the spinal muscles. This can cause increased soft tissue retraction, which generates more pain after the operation.
Special Techniques
Dr Steel performs lumbar decompression and fusion using a specialised minimally invasive technique in most cases. The aim is to reduce disruption to the normal tissues and allow a more rapid return to normal function.
Dr Steel uses much smaller exposures in minimally invasive spine surgery than in traditional spine surgery. The goals of the surgery remain the same – i.e. to decompress the affected nerves and spinal cord and to fuse or replace arthritic and painful joints.
Because of the inaccessibility of the spine, traditional spine operations involve exposing and pulling back skin, muscles and ligaments. This retraction can hamper recovery by causing pain and swelling.
Minimally invasive spine procedures require less exposure and retraction in order to conduct the surgery. Minimally invasive spine fusions allow surgeons to place titanium hardware through a narrow path that is created by separating muscles rather than cutting and retracting.
Early in 2009, Dr Steel performed the first percutaneous spine fusion using image fusion stereotactic navigation combining pre-operative CT scans with intra-operative x-rays to make the surgery more accurate and safer for the patient.
Conditions suitable for MISS
The majority of spine surgery is still performed via an open procedure. However, advances in surgical techniques, stereotactic navigation and improved spinal fixation devices have made minimally invasive spine surgery safer and more effective for treating many conditions.
The following spinal conditions are suitable for MISS techniques:
- Cervical and lumbar herniated discs
- Degenerative scoliosis
- Cervical and lumbar spinal stenosis and lateral recess stenosis
- Spondylolisthesis